Dry Needling for Plantar Fasciitis
Plantar fasciitis is a debilitating condition that affects the bottom of the foot, causing intense heel pain and discomfort. It is one of the most common orthopedic complaints, especially among athletes, runners, and individuals who spend a significant amount of time on their feet. Traditional treatments range from rest and stretching to medication and surgery. However, many people continue to suffer despite these interventions.
Dry needling has emerged as an effective treatment method targeting the root cause of pain—myofascial trigger points in the muscles. By inserting thin needles into specific areas of muscle tension, dry needling can provide significant relief for those struggling with plantar fasciitis. This post delves into how dry needling works, its benefits, and how it compares to other treatment options.
Key Points
Misdiagnosis of Heel Pain: Many cases of heel pain are misdiagnosed as plantar fasciitis when they are actually caused by myofascial trigger points.
Effectiveness of Dry Needling: Targeting trigger points in the foot and calf muscles, dry needling offers significant pain relief and improved foot function.
Research Support: Clinical studies demonstrate that dry needling can reduce pain in both the short and long term.
Dry Needling vs. Acupuncture: While both use needles, dry needling focuses on muscular trigger points, whereas acupuncture is based on traditional Chinese medicine principles.
Safety and Side Effects: Dry needling is generally safe with mild, temporary side effects.
Cost Considerations: Dry needling can be a cost-effective treatment compared to other interventions.
Overview of Plantar Fasciitis
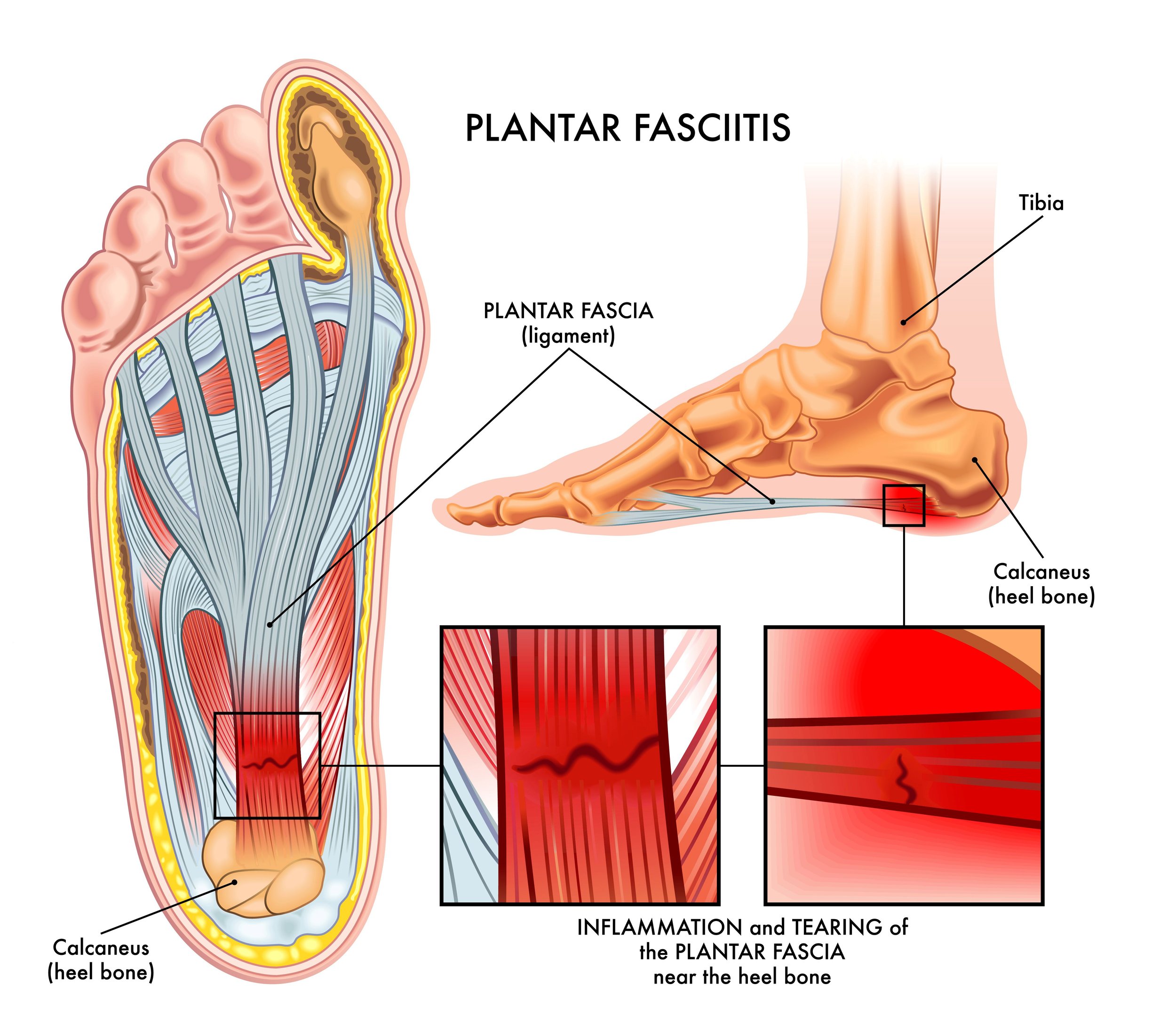
Plantar fasciitis involves inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. This condition is often characterized by stabbing pain near the heel, especially during the first steps in the morning. It affects approximately 10% of the population at some point in their lives.
The plantar fascia acts like a shock-absorbing bowstring, supporting the arch of the foot. When tension and stress on this bowstring become too great, small tears can occur in the fascia. Repetitive stretching and tearing can cause the fascia to become irritated or inflamed, leading to pain.
However, not all heel pain is due to plantar fascia inflammation. Studies have shown that many cases are actually caused by tight or dysfunctional muscles in the lower leg and foot, developing trigger points that refer pain to the heel. Misdiagnoses are common without proper imaging or thorough clinical evaluation, leading to ineffective treatments.
Plantar Fasciitis Symptoms
The symptoms of plantar fasciitis can vary in intensity and duration. Common signs and symptoms include:
Sharp Heel Pain: A stabbing pain at the bottom of the heel, often worse with the first steps after waking up.
Increased Pain After Rest: Discomfort that intensifies after prolonged periods of sitting or inactivity.
Pain After Exercise: Pain that flares up after, not during, physical activity.
Foot Stiffness: Tightness in the foot arch, making it difficult to flex the foot upward.
Tenderness: Sensitivity when pressing on the heel or along the arch of the foot.
Mild Swelling: Occasional swelling or redness in the heel area.
Limping: Altered gait to avoid putting pressure on the affected heel.
These symptoms can significantly impact daily activities, making it challenging to walk, exercise, or stand for extended periods. Early intervention is crucial to prevent the condition from becoming chronic.
Biomechanics and Plantar Fasciitis
Understanding the biomechanics of the foot is essential in addressing plantar fasciitis. The foot is a complex structure comprising bones, muscles, tendons, and ligaments that work together to provide support and mobility. Any imbalance or dysfunction in this system can lead to excessive strain on the plantar fascia.
Factors Contributing to Plantar Fasciitis Pain:
Overpronation: Excessive inward rolling of the foot during walking or running increases stress on the plantar fascia.
High Arches or Flat Feet: Abnormal foot arches alter weight distribution, leading to additional strain.
Tight Calf Muscles: Limited ankle dorsiflexion due to tight calf muscles places more tension on the plantar fascia during gait.
Improper Footwear: Lack of proper support or cushioning can exacerbate biomechanical issues.
Muscle Imbalances: Weakness in the foot and ankle muscles affects stability and gait mechanics.
Addressing biomechanical factors through therapies like dry needling, stretching, and strengthening exercises can alleviate symptoms and prevent recurrence.
Plantar Fasciitis Treatments
Treatment approaches for plantar fasciitis aim to reduce pain, decrease inflammation, and promote healing. They include both conservative and more invasive options.
Conservative Treatments:
Rest and Activity Modification: Limiting activities that aggravate the condition to allow the fascia to heal.
Ice Therapy: Applying ice packs to the affected area to reduce inflammation and numb pain.
Stretching Exercises: Focusing on the plantar fascia, Achilles tendon, and calf muscles to improve flexibility.
Physical Therapy: Incorporating manual therapy and modalities to relieve pain and improve function.
Orthotic Devices: Using custom-made shoe inserts or heel pads to provide support and correct biomechanical issues.
Night Splints: Wearing splints during sleep to maintain a stretched position of the plantar fascia and Achilles tendon.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen to alleviate pain and reduce inflammation.
Acupuncture and Dry Needling: Utilizing needles to stimulate healing and release muscle tension.
Invasive Treatments:
Extracorporeal Shock Wave Therapy (ESWT): Applying sound waves to stimulate tissue healing.
Corticosteroid Injections: Injecting steroids into the affected area to reduce severe inflammation.
Platelet-Rich Plasma (PRP) Injections: Using concentrated platelets from the patient's blood to promote tissue repair.
Surgery: In rare cases, surgical intervention may be necessary to detach the plantar fascia from the heel bone.
While many patients respond well to conservative treatments, others may require additional interventions. Dry needling offers an effective alternative, especially for those who have not found relief through traditional methods.
Plantar Fasciitis Trigger Points
Myofascial trigger points (MTrPs) are hyperirritable spots in skeletal muscle that are associated with palpable nodules in taut bands of muscle fibers. These trigger points can refer pain to other areas, often mimicking or contributing to plantar fasciitis symptoms.
Key Muscles with Trigger Points Related to Heel Pain:
Gastrocnemius (Calf Muscle):
Trigger Points: Located in the upper part of the calf muscle.
Pain Referral: Can cause pain in the heel and sole of the foot.
Contributing Factors: Overuse, improper footwear, or sudden increase in activity.
Soleus (Deep Calf Muscle):
Trigger Points: Found in the lower calf near the Achilles tendon.
Pain Referral: Refers pain to the heel and can mimic plantar fasciitis.
Contributing Factors: Prolonged standing, uphill walking, or inadequate stretching.
Quadratus Plantae (Foot Muscle):
Trigger Points: Located on the bottom of the foot near the heel.
Pain Referral: Causes deep heel pain, especially during weight-bearing activities.
Contributing Factors: Excessive foot pronation or tight footwear.
Abductor Hallucis:
Trigger Points: Along the inside of the foot arch.
Pain Referral: Medial heel and arch pain.
Contributing Factors: Flat feet, overpronation, or excessive strain.
Flexor Digitorum Brevis:
Trigger Points: In the middle of the sole of the foot.
Pain Referral: Pain along the arch extending towards the toes.
Contributing Factors: Toe gripping, high heels, or overuse.
Addressing Trigger Points:
Treating these trigger points can alleviate referred pain and reduce tension on the plantar fascia. Techniques include:
Dry Needling: Directly targeting trigger points to release muscle tension.
Manual Therapy: Massage and myofascial release techniques.
Stretching: Specific stretches to lengthen tight muscles.
Strengthening Exercises: Improving muscle balance and function.
By focusing on these muscular components, practitioners can provide a more comprehensive treatment for heel pain.
Dry needling for plantar fasciitis
Dry Needling for Plantar Fasciitis
Dry needling involves the insertion of thin, sterile needles into myofascial trigger points to provoke a healing response in soft tissues. Unlike acupuncture, which is based on traditional Chinese medicine, dry needling is rooted in Western medical principles and focuses on musculoskeletal pain and dysfunction.
How Dry Needling Works:
Mechanical Disruption: Inserting the needle disrupts the integrity of the dysfunctional tissue, causing a localized twitch response that can release muscle tension.
Neurophysiological Effects: Stimulates nerve fibers, altering pain perception and reducing nociceptive inputs.
Chemical Changes: Promotes the release of endogenous opioids and neurotransmitters that modulate pain.
Increased Blood Flow: Enhances circulation to the affected area, promoting healing.
Benefits for Plantar Fasciitis:
Targeted Treatment: Directly addresses trigger points contributing to heel pain.
Non-Invasive: Minimally invasive with low risk compared to surgical options.
Quick Results: Many patients experience pain relief after a few sessions.
Complementary Therapy: Can be used alongside other treatments like physical therapy or orthotics.
Treatment Process:
During a dry needling session for plantar fasciitis, the practitioner will:
Assessment: Identify specific trigger points in the calf and foot muscles.
Needle Insertion: Gently insert needles into the trigger points.
Manipulation: May manipulate the needles to elicit a twitch response.
Duration: Needles may or may not be left in place for a short period, usually a few minutes.
Aftercare: Provide guidance on stretches or activities to enhance treatment effectiveness.
Ways Dry Needling Helps Plantar Fasciitis
Dry needling offers multiple therapeutic benefits for individuals suffering from plantar fasciitis:
Reduces Muscle Tightness: Relieves tension in the calf and foot muscles, decreasing strain on the plantar fascia.
Alleviates Pain: Interrupts pain signals and reduces sensitivity in the affected area.
Improves Range of Motion: Restores flexibility in tight muscles, enhancing mobility.
Enhances Healing: Stimulates the body's natural healing processes by increasing blood flow and reducing inflammation.
Addresses Underlying Causes: Targets the root muscular issues rather than just masking symptoms.
By integrating dry needling into a comprehensive treatment plan, patients can experience significant improvements in pain levels and overall foot function.
Research on Dry Needling for Plantar Fasciitis
Several studies have investigated the efficacy of dry needling for plantar fasciitis, demonstrating promising results.
Eftekharsadat et al. (2016):
Study Design: Single-blinded randomized clinical trial involving patients with chronic heel pain.
Findings:
Significant reduction in pain severity after dry needling treatments.
Improved foot function and patient satisfaction.
Conclusion: Dry needling is an effective intervention for chronic plantar fasciitis.
Llurda-Almuzara et al. (2021):
Study Design: Systematic review and meta-analysis of multiple randomized controlled trials.
Findings:
Moderate to long-term pain relief in patients receiving dry needling.
Notable improvements in pain intensity and functional disability.
Conclusion: Supports dry needling as a beneficial treatment for plantar heel pain.
He & Ma (2017):
Study Design: Meta-analysis of seven randomized controlled trials focusing on trigger point dry needling.
Findings:
Significant pain reduction compared to control groups.
Enhanced treatment outcomes when combined with other therapies.
Conclusion: Dry needling is effective for managing plantar heel pain associated with trigger points.
These studies highlight the potential of dry needling as a viable option for those who have not responded to conventional treatments.
Dry Needling vs. Acupuncture for Plantar Fasciitis
While dry needling and acupuncture both involve the use of needles, they differ in methodology, philosophy, and application.
Dry Needling:
Focus: Targets myofascial trigger points to alleviate muscle tension and pain.
Basis: Rooted in Western medicine principles, emphasizing anatomy and neurophysiology.
Application: Used primarily for musculoskeletal conditions and pain management.
Practitioners: Typically performed by physical therapists, chiropractors, and some acupuncturists trained in dry needling techniques.
Acupuncture:
Focus: Stimulates specific points along meridians to balance the body's energy (Qi).
Basis: Founded on Traditional Chinese Medicine (TCM) concepts.
Application: Addresses a wide range of conditions, including pain, digestive issues, and stress.
Practitioners: Performed by licensed acupuncturists.
Combined Approach:
Benefits:
Provides a holistic treatment by addressing both physical and energetic aspects.
May enhance overall effectiveness and patient outcomes.
Practitioner Qualifications:
Some acupuncturists are trained in dry needling, offering a comprehensive skill set.
Allows for personalized treatment plans tailored to individual needs.
Choosing between dry needling and acupuncture may depend on personal preference, practitioner availability, and specific treatment goals.
Dry Needling for Plantar Fasciitis Side Effects
Dry needling is generally considered safe when performed by a qualified professional. Side effects are typically mild and short-lived.
Common Side Effects:
Soreness: Temporary muscle soreness or aching at the needle insertion sites.
Bruising: Minor bruising may occur due to needle penetration.
Fatigue: Some patients report feeling tired after treatment.
Lightheadedness: Rarely, patients may feel dizzy or lightheaded.
Rare Side Effects:
Infection: Minimal risk when proper sterilization techniques are used.
Nerve Damage: Extremely rare but possible if needles are improperly placed.
Pneumothorax: A collapsed lung can occur if needling is done incorrectly in the thoracic region (not typically a concern for plantar fasciitis treatment).
Precautions:
Professional Training: Ensure the practitioner is licensed and has appropriate training in dry needling.
Medical History: Discuss any medical conditions, such as bleeding disorders or pregnancy, with the practitioner.
Aftercare: Follow any post-treatment instructions to minimize side effects.
Most side effects resolve within 24 to 48 hours, and patients can typically resume normal activities immediately after treatment.
Cost of Dry Needling for Plantar Fasciitis
The cost of dry needling varies based on several factors, including geographic location, practitioner expertise, and the number of sessions required.
Average Costs:
Per Session: Typically ranges from $100 to $400.
Total Treatment: Depends on the number of sessions, which can vary from 3 to 6 or more.
Insurance Coverage:
Acupuncture Coverage: Some insurance plans cover acupuncture, which may include acupuncture or dry needling if performed by a licensed acupuncturist.
Physical Therapy: Dry needling may be covered if performed by a physical therapist as part of a rehabilitation program.
Verification: Patients should check with their insurance providers to determine coverage specifics. Some providers like Morningside Acupuncture may be out-of-network with all insurance providers.
Cost-Effectiveness:
Compared to Surgery: Significantly less expensive than surgical interventions.
Long-Term Savings: Effective treatment can reduce the need for ongoing medication or therapy.
Value: Investing in dry needling can lead to improved quality of life and reduced pain.
Patients should discuss costs and treatment plans with their practitioners to make informed decisions.
Conclusion
Plantar fasciitis is a common and often debilitating condition that can significantly impact daily life. Traditional treatments may provide relief for some, but others continue to struggle with persistent heel pain. Dry needling offers a promising alternative by targeting the myofascial trigger points that contribute to the discomfort associated with plantar fasciitis.
By focusing on the underlying muscular issues rather than just the symptoms, dry needling addresses one of the root causes of heel pain. The technique releases muscle tension, reduces inflammation, and promotes natural healing processes. Supported by scientific research, dry needling has demonstrated effectiveness in reducing pain and improving foot function, making it a valuable addition to comprehensive treatment plans.
Whether you're an athlete, someone who spends long hours on your feet, or an individual seeking relief from chronic heel pain, dry needling may offer the solution you've been searching for. Its minimally invasive nature, combined with generally mild and temporary side effects, makes it an accessible and safe option for many patients.
If traditional treatments have not provided the desired relief, consider exploring dry needling as part of your recovery journey. Collaborating with a qualified practitioner can help tailor a treatment plan that addresses your specific needs and enhances your overall well-being.
Frequently Asked Questions (FAQ)
Does dry needling for plantar fasciitis hurt?
Dry needling involves inserting thin needles into specific muscle trigger points, which may cause a brief, sharp sensation. Most patients describe the discomfort as minimal and tolerable. The sensation often feels like a slight muscle cramp or twitch when the needle stimulates the trigger point. Any discomfort typically subsides quickly, and practitioners take care to ensure patient comfort throughout the procedure.
How painful is dry needling for plantar fasciitis?
The level of pain experienced during dry needling varies among individuals. Some patients report feeling a mild aching or pressure, while others may experience a quick muscle twitch or cramp sensation. The needles used are very thin, much like those used in acupuncture, and the procedure is generally well-tolerated. Any post-treatment soreness is usually mild and temporary, resolving within a day or two.
What is dry needling for plantar fasciitis?
Dry needling is a therapeutic technique where trained practitioners insert fine needles into specific myofascial trigger points—tight bands or knots within a muscle. For plantar fasciitis, dry needling targets trigger points in the foot and calf muscles that contribute to heel pain. The goal is to release muscle tension, reduce pain, and restore normal muscle function, thereby alleviating stress on the plantar fascia.
Does dry needling work for plantar fasciitis?
Yes, research indicates that dry needling can be an effective treatment for plantar fasciitis. Studies have shown significant reductions in pain and improvements in foot function following dry needling treatments. By targeting and releasing trigger points in the muscles contributing to heel pain, dry needling addresses one of the underlying causes of plantar fasciitis.
How many dry needling sessions are needed for plantar fasciitis?
The number of sessions required varies depending on the severity of the condition and individual response to treatment. On average, patients may need between 3 to 6 sessions spaced over several weeks for optimal results. Your practitioner will assess your condition and develop a personalized treatment plan tailored to your needs.
Is dry needling good for plantar fasciitis?
Dry needling is considered a beneficial treatment option for plantar fasciitis, especially for those who have not found relief through conventional therapies. It effectively reduces muscle tension, decreases pain, and improves mobility. When combined with other treatments like stretching and strengthening exercises, dry needling can enhance overall recovery.
How does dry needling work for plantar fasciitis?
Dry needling works by inserting thin needles into myofascial trigger points within the muscles of the foot and calf. This process stimulates a local twitch response, which helps release tight muscle bands. The mechanical and neurological effects of dry needling reduce muscle tension, improve blood flow, and interrupt pain signals, thereby alleviating heel pain associated with plantar fasciitis.
How effective is dry needling for plantar fasciitis?
Dry needling has been shown to be effective in reducing pain and improving function in patients with plantar fasciitis. Clinical studies and meta-analyses have demonstrated significant improvements in pain levels and foot function following dry needling treatments. Its effectiveness can be enhanced when combined with other therapies like physical therapy and exercise.
Is dry needling effective for plantar fasciitis?
Yes, dry needling is an effective treatment modality for plantar fasciitis. By directly targeting the muscle trigger points that contribute to heel pain, it offers relief from symptoms and addresses underlying muscular issues. Research supports its use as part of a comprehensive treatment plan for plantar fasciitis.
Is dry needling safe for plantar fasciitis?
When performed by a qualified and trained practitioner, dry needling is considered safe for treating plantar fasciitis. The procedure uses sterile, single-use needles, and practitioners follow strict protocols to minimize risks. Side effects are generally mild and may include temporary soreness or bruising at the needle sites. Serious complications are rare.
Related Articles:
Acupuncture for Calf Trigger Points
Combining Acupuncture and Physical Therapy
Acupuncture for Foot Pain
Contact Us to Schedule an Appointment
Ready to explore dry needling for plantar fasciitis relief? Our experienced team at Morningside Acupuncture is here to help. We specialize in both dry needling and acupuncture, providing comprehensive care to address your unique needs.
Over to you
If you liked this article, please share with friends and family who may be suffering with plantar fasciitis or heel pain.
Sources:
Travell, J. G., Simons, D. G. (1993). Myofascial pain and dysfunction: The trigger point manual. London: Lippincott Williams & Wilkins.
Biel, A., & Dorn, R. (2010). Trail guide to the body: A hands-on guide to locating muscles, bones and more. Boulder, CO: Books of Dicovery.
Eftekharsadat, B., Babaei-Ghazani, A., & Zeinolabedinzadeh, V. (2016). Dry needling in patients with chronic heel pain due to plantar fasciitis: A single-blinded randomized clinical trial. Medical Journal of the Islamic Republic of Iran, 30, 401. Link
Llurda-Almuzara, L., et al. (2021). Is dry needling effective for the management of plantar heel pain or plantar fasciitis? An updated systematic review and meta-analysis. Pain Medicine, 22(7), 1630–1641. Link
He, C., & Ma, H. (2017). Effectiveness of trigger point dry needling for plantar heel pain: A meta-analysis of seven randomized controlled trials. Journal of Pain Research, 10, 1933–1942. Link
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.