Study Finds Acupuncture May Improve IBS Symptoms
Acupuncture Shows Promise in Treating Refractory Irritable Bowel Syndrome: A Randomized Controlled Trial
A recent 2024 study has found that acupuncture may significantly improve symptoms in patients with refractory irritable bowel syndrome (IBS) when combined with usual care. Published in Frontiers of Medicine (2024), the study offers new evidence supporting acupuncture as a safe and effective adjunctive treatment for IBS patients who have not responded to conventional therapies. This finding provides hope for individuals struggling with persistent IBS symptoms despite standard medical interventions.
Key Points
Significant Symptom Reduction: Patients receiving acupuncture experienced a substantial decrease in IBS Symptom Severity Scale (IBS-SSS) scores compared to those receiving sham acupuncture.
Enhanced Quality of Life: Participants reported improvements in various aspects of quality of life, including reduced anxiety and better social functioning.
Sustained Benefits: The symptom relief achieved with acupuncture was maintained during a four-week follow-up period after the treatment ended.
Safe Treatment Option: No serious adverse events were reported, indicating that acupuncture is a safe therapy for refractory IBS.
High Response Rate: A notable 90.6% of patients in the acupuncture group showed clinically significant improvements.
Study Overview
Background
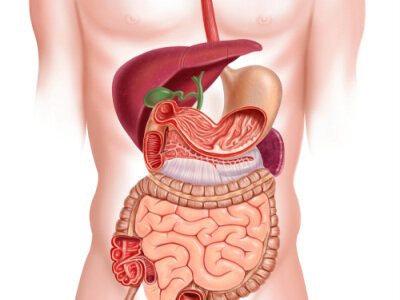
Irritable bowel syndrome affects up to 20% of the global population, causing symptoms like abdominal pain, bloating, and altered bowel habits that can severely impact quality of life. Refractory IBS refers to cases where patients do not respond adequately to standard treatments such as dietary changes and medications. This lack of effective options often leads patients to explore alternative therapies like acupuncture to manage their symptoms.
Objective
The study aimed to evaluate the efficacy and safety of acupuncture compared to sham acupuncture in patients with refractory IBS, all while they continued their usual care. Researchers wanted to determine if acupuncture could provide additional benefits in symptom relief and quality of life for these patients.
Methodology
This multicenter, randomized, sham-controlled trial involved 170 adults aged 18 to 70 with refractory IBS. Participants were randomly assigned to either the acupuncture group or the sham acupuncture group, each with 85 patients. Both groups continued their prescribed medications and dietary interventions throughout the study.
Intervention Details:
Acupuncture Group: Received 12 sessions of true acupuncture over four weeks (three sessions per week), targeting specific acupoints relevant to IBS symptoms.
Sham Acupuncture Group: Received 12 sessions of superficial needling at non-acupuncture points without manual stimulation, serving as a control to account for placebo effects.
Outcome Measures:
Primary Outcome: Change in IBS Symptom Severity Scale (IBS-SSS) scores from baseline to week 4.
Secondary Outcomes: Assessments of quality of life (IBS-QOL), Work and Social Adjustment Scale (WSAS), anxiety and depression scales (SAS and SDS), and stool frequency and consistency.
Blinding
To maintain the integrity of the results, patients, outcome assessors, and statisticians were blinded to group assignments. Acupuncturists were not blinded due to the nature of the intervention.
Key Findings
Symptom Severity Reduction
Patients who received true acupuncture showed a significant reduction in IBS symptom severity:
IBS-SSS Scores:
Acupuncture Group: Mean reduction of 140.0 points from baseline.
Sham Group: Mean reduction of 64.4 points from baseline.
Between-Group Difference: 75.6 points (95% CI: 55.8 to 95.4; P < .001).
This indicates that acupuncture significantly alleviates IBS symptoms beyond the placebo effect.
Clinical Response Rate
A clinically significant improvement was defined as a reduction of at least 50 points in IBS-SSS scores:
Acupuncture Group: 90.6% of patients achieved this level of improvement.
Sham Group: 44.7% reached the same benchmark.
Between-Group Difference: 45.9% (95% CI: 31.7% to 57.7%; P < .001).
These results underscore the effectiveness of acupuncture in providing meaningful symptom relief.
Quality of Life Improvements
Patients in the acupuncture group reported significant improvements in quality of life:
IBS-QOL Scores:
Enhanced overall quality of life, including areas like emotional well-being and social functioning.
Between-Group Difference: 8.4 points improvement in favor of acupuncture (95% CI: 4.6 to 12.2; P < .001).
Sustained Benefits
The benefits of acupuncture persisted beyond the treatment period:
Follow-Up Assessments: At weeks 6 and 8 post-treatment, patients maintained lower IBS-SSS scores compared to the sham group.
Symptom Relief: This suggests that acupuncture may have lasting effects on gastrointestinal function and patient well-being.
Safety Profile
Safety was a key consideration:
Adverse Events:
Acupuncture Group: Minor adverse events occurred in 9 out of 85 patients, mainly transient subcutaneous hematoma.
Sham Group: Minor events reported in 4 out of 85 patients.
No Serious Adverse Events: Neither group experienced serious complications, indicating that acupuncture is a safe treatment option for refractory IBS.
Study Strengths
The study's design and execution contribute to the reliability of its findings:
Robust Design: The multicenter, randomized, sham-controlled trial enhances validity and generalizability.
Effective Blinding: Patients, outcome assessors, and statisticians were blinded, reducing potential biases.
Adequate Sample Size: Including 170 participants provided sufficient power to detect significant differences.
Use of Validated Measures: Standardized instruments like the IBS-SSS and IBS-QOL were employed.
High Adherence and Low Dropout Rate: Only 6% of participants dropped out, indicating good engagement.
Sustained Follow-Up: The four-week follow-up allowed assessment of the durability of acupuncture's effects.
Safety Monitoring: Regular assessments ensured patient safety throughout the study.
Study Weaknesses
Some limitations were noted:
Single-Blind Design: Acupuncturists were not blinded, which could introduce bias.
Potential Placebo Effect: Creating a completely inert sham acupuncture procedure is challenging, possibly affecting control group outcomes.
Cultural Context: Conducted in China, cultural perceptions of acupuncture might limit generalizability to other populations.
IBS Subtype Representation: Most participants had IBS with predominant diarrhea (IBS-D), limiting applicability to other subtypes like IBS with constipation (IBS-C).
Short Follow-Up: A longer follow-up could better assess the long-term efficacy of acupuncture.
Blinding Integrity: Some patients might have guessed their group allocation based on sensations during treatment.
Lack of Objective Measures: No physiological assessments were included to corroborate patient-reported outcomes.
Implications for Practice
Effective Adjunctive Therapy
Acupuncture offers an additional option for patients not responding to conventional treatments, providing symptom relief without medication side effects. This non-pharmacological approach can be particularly appealing to those seeking alternative or complementary therapies.
Patient-Centered Care
Improvements extend beyond physical symptoms to overall well-being. Patients experienced better daily functioning and reduced anxiety, which are crucial aspects of managing a chronic condition like IBS.
Integration into Treatment Plans
Healthcare providers might consider incorporating acupuncture into comprehensive IBS management:
Holistic Approach: Combining acupuncture with dietary advice, medications, and psychological interventions can address multiple facets of IBS.
Accessibility: Acupuncture is widely available and can be administered by trained professionals in various healthcare settings.
Understanding Acupuncture's Role
Potential Mechanisms
While not fully understood, several theories explain acupuncture's efficacy in IBS:
Neuromodulation: May influence the gut-brain axis, modulating neurotransmitters and hormones that affect gastrointestinal function.
Stress Reduction: Can alleviate stress and anxiety, which are known to exacerbate IBS symptoms.
Anti-Inflammatory Effects: Might reduce local inflammation in the gastrointestinal tract, contributing to symptom relief.
Addressing the Placebo Effect
The use of sham acupuncture helps differentiate true therapeutic effects from placebo responses. Despite the challenges in creating a completely inert control, the significant differences observed suggest that acupuncture's benefits are genuine.
Conclusion
This study provides strong evidence that acupuncture is an effective and safe adjunctive treatment for patients with refractory IBS. By significantly reducing symptoms and improving quality of life, acupuncture emerges as a promising option for those seeking relief from this challenging condition. Healthcare providers should consider acupuncture as part of a comprehensive treatment strategy, especially for patients who have not responded to conventional therapies.
Over to you
If you liked this article, please share with friends and family who may want to learn more about acupuncture for refractory IBS.
Sources:
Zhao, J., Zheng, H., Wang, X., Wang, X., Shi, Y., Xie, C., Tao, Q., Li, D., Sun, J., Tian, J., Gao, J., Liu, H., Shi, S., Ni, J., Xue, R., Hu, H., Chen, M., Yu, S., & Li, Z. (2024). Efficacy of acupuncture in refractory irritable bowel syndrome patients: a randomized controlled trial. Frontiers of medicine, 18(4), 678–689. https://doi.org/10.1007/s11684-024-1073-7
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.