Acupuncture for Patellofemoral Pain
Runner with knee taped up due to runner’s knee or patellorfemoral pain syndrome (PFPS)
Acupuncture Can Provide An Effective Solution for Runner's Knee
Acupuncture has long been known for its healing capabilities in the treatment of various sports injuries and ailments. One such condition that can significantly benefit from acupuncture is Patellofemoral Pain Syndrome (PFPS), commonly referred to as Runner's Knee.
What is Patellofemoral Pain Syndrome (PFPS)?
PFPS is a common overuse injury among runners, hence its nickname "Runner's Knee." The syndrome is characterized by diffuse pain around the kneecap (patella). It can be caused by muscular imbalances or misalignment of the knee joint, leading to the patella rubbing against the femur (thighbone) during movement. This friction can result in inflammation, pain, and, if left untreated, can contribute to long-term knee damage. Research has shown that this condition is especially prevalent among female athletes and individuals with a higher body mass index.
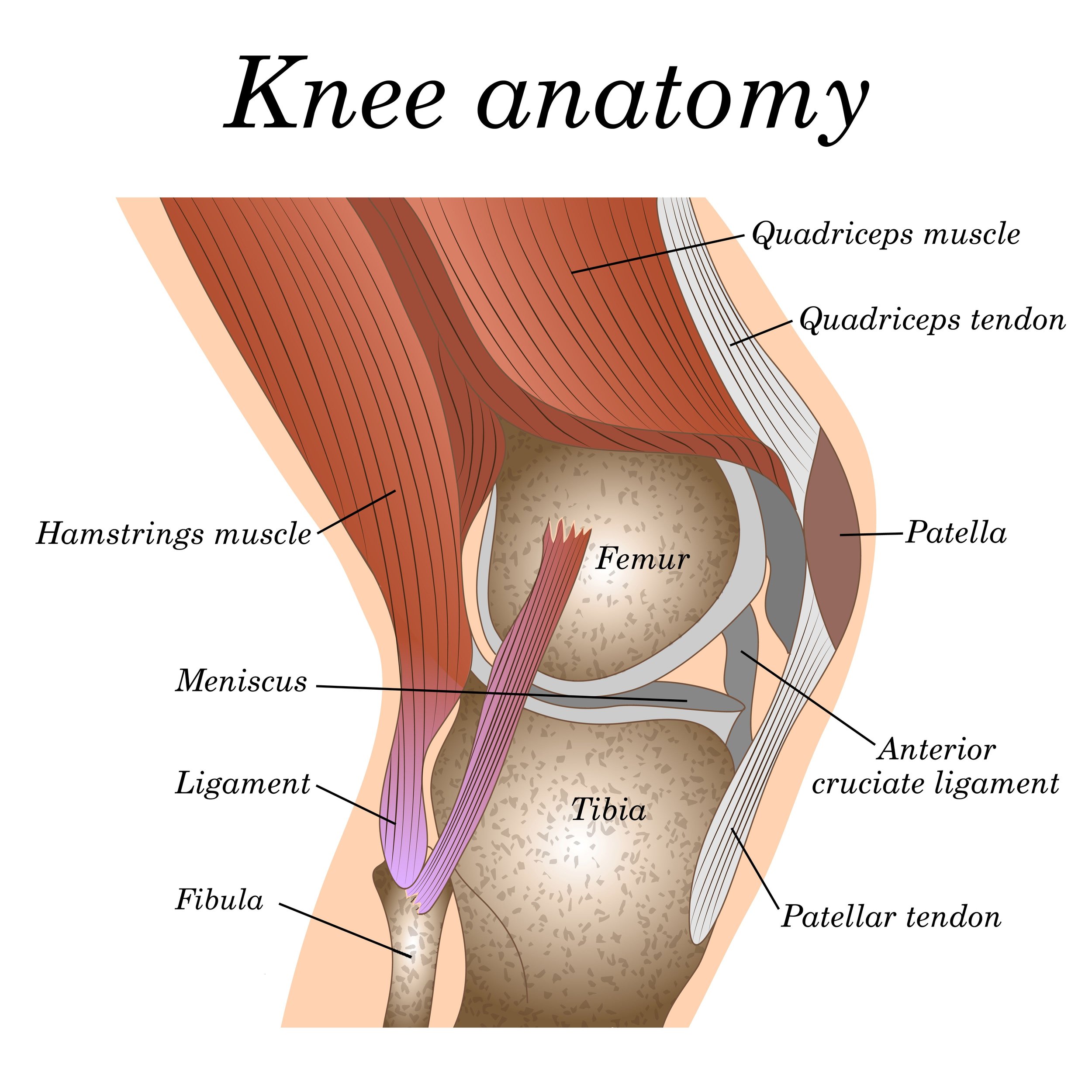
The Anatomy of the Knee and PFPS
The knee joint is a complex structure composed of bones, muscles, tendons, and ligaments. In the context of PFPS, key muscles include the quadriceps, particularly the vastus medialis obliquus (VMO), and the hamstrings, both of which play a crucial role in knee stability and movement. Weakness or imbalance in these muscles can result in excessive lateral tracking of the patella, contributing to PFPS. Studies have highlighted the importance of these muscles and the benefits of strengthening exercises in the management of PFPS.
Knee anatomy
Acupuncture for PFPS
Acupuncture can be an excellent adjunct to a comprehensive treatment plan for PFPS. By targeting specific acupuncture points around the knee and along the pathways of affected muscles, acupuncture can help relieve pain, reduce inflammation, and promote healing. Moreover, acupuncture can help balance muscle function, potentially addressing some of the muscular imbalances contributing to PFPS.
Research supports the efficacy of acupuncture for knee pain, including PFPS. A 2018 systematic review and meta-analysis of randomized controlled trials found that acupuncture significantly improved pain and function in patients with chronic knee pain.
In our clinic at Morningside Acupuncture, we often combine traditional acupuncture with trigger point dry needling for effective relief of PFPS. Dry needling can be particularly useful in deactivating trigger points in the quadriceps and hamstrings, which can help alleviate pain and improve muscular function.
Dry Needling for PFPS
A growing body of evidence supports the use of dry needling as a primary intervention for PFPS. Dry needling, an acupuncture technique, is a therapy that involves inserting fine needles into myofascial trigger points to alleviate pain and restore function.
In a study published in The Journal of Orthopaedic & Sports Physical Therapy, the authors found that dry needling was effective in reducing pain and improving function in patients with PFPS along with physical therapy. The researchers attributed some of these improvements to the mechanism of dry needling, which helps alleviate trigger points and thereby corrects the underlying muscular imbalances contributing to PFPS.
Another research article in The Journal of Clinical medicine found that dry needling resulted in significant improvements in pain and function for patients with chronic patellofemoral pain syndrome. The study highlighted dry needling's role in reducing muscle tension and facilitating muscle relaxation, which can help restore proper patellar tracking and alleviate PFPS symptoms.
A 2023 research study found that dry needling for trigger points was notably more effective in diminishing pain and improving function in individuals with patellofemoral pain syndrome compared to traditional therapeutic methods.
At Morningside Acupuncture, our experienced practitioners employ dry needling as part of a comprehensive treatment approach for PFPS. By targeting the specific trigger points associated with your knee pain, we can help restore balance to the affected muscles, correct your movement mechanics, and ultimately, alleviate the pain and dysfunction associated with PFPS.
What Causes PFPS?
Patellofemoral Pain Syndrome (PFPS), also known as Runner's Knee, often stems from overuse or excessive stress on the knee joint. This condition is common among athletes who participate in high-impact activities such as running, jumping, or cycling. However, it is also seen among non-athletes, caused by repetitive strains on the knee during everyday activities such as climbing stairs or sitting for prolonged periods with the knees bent.
PFPS is primarily a biomechanical issue. The patella, or kneecap, is situated within the femoral groove in the femur. It is designed to glide smoothly up and down this groove during movement. A delicate equilibrium of forces exerted by various muscles and soft tissues ensures that the patella remains in its proper place. However, disruptions to this balance can lead the patella to deviate from its optimal path, resulting in inflammation and pain.
Key to maintaining proper patellar tracking is the interplay of several muscles. The quadriceps muscle group, specifically the vastus medialis obliquus (VMO) and vastus lateralis, have significant roles. The VMO pulls the patella inward, while the vastus lateralis exerts an outward force. An imbalance, often due to a weak VMO or a tight vastus lateralis, can result in the patella being pulled too far to the outside, causing irritation and pain.
In addition, the hip muscles, particularly the gluteus medius, are crucial. They provide stability to the hips and pelvis during movement. Weak or dysfunctional hip muscles can alter the alignment of the entire leg, including the knee, which can contribute to PFPS.
Overuse, a sudden increase in training intensity or volume, poor movement mechanics, or even anatomical factors (like flat feet) can all contribute to the development of PFPS.
Understanding Trigger Points in PFPS (Patellofemoral Pain Syndrome)
In their groundbreaking work, Travell and Simons extensively explored the impact of myofascial trigger points on various musculoskeletal conditions, including PFPS. They observed that trigger points—hyperirritable nodules found within tight bands of muscle fibers—can generate pain patterns that mimic several common musculoskeletal conditions, including PFPS.
For PFPS specifically, Travell and Simons identified several muscles prone to developing trigger points that can cause or contribute to knee pain. These include the quadriceps group, especially the vastus medialis and vastus lateralis, as well as the hamstrings, gastrocnemius, popliteus, and even the hip muscles such as the gluteus medius and hip adductors.
For instance, active trigger points in the vastus medialis can produce pain felt along the inside of the knee, while trigger points in the vastus lateralis can cause pain felt on the outer side of the knee. Both scenarios could contribute to patellar maltracking and the pain patterns associated with PFPS.
Moreover, trigger points in the hip muscles, which play a crucial role in stabilizing the hip and knee joints during movement, could indirectly contribute to PFPS by altering movement mechanics. Specifically, trigger points in the gluteus medius, a key stabilizer of the hip, could lead to increased stress on the knee joint during activity.
Importantly, Travell and Simons highlight that treating these trigger points can provide significant relief from the pain and dysfunction caused by PFPS. In the hands of skilled practitioners at Morningside Acupuncture, trigger point therapies, such as dry needling—an acupuncture technique—are used to effectively deactivate these trigger points, alleviate pain, and restore proper movement mechanics.
Acupuncture and Dry Needling as a First Line PFPS Treatment
Despite PFPS being a common condition, it often goes undiagnosed or misdiagnosed, leading to ineffective treatments. However, acupuncture and dry needling can provide an effective first line of treatment. A conservative management approach, including acupuncture, can be successful in managing PFPS, reducing the need for invasive surgical procedures.
If you or someone you know is suffering from PFPS, schedule an appointment with us today. Our experienced practitioners can provide a comprehensive evaluation and treatment plan tailored to your specific needs.
Over to you
If you liked this article, please share with friends and family who may be suffering with patellofemoral pain syndrome.
Sources:
Travell, J. G., Simons, D. G. (1993). Myofascial pain and dysfunction: The trigger point manual. London: Lippincott Williams & Wilkins.
Biel, A., & Dorn, R. (2010). Trail guide to the body: A hands-on guide to locating muscles, bones and more. Boulder, CO: Books of Dicovery.
Janda, Vladimír. “Muscle Function Testing.” (1983).
Pappas, E., & Wong-Tom, W. M. (2012). Prospective Predictors of Patellofemoral Pain Syndrome: A Systematic Review With Meta-analysis. Sports health, 4(2), 115–120. https://doi.org/10.1177/1941738111432097
Neal, B. S., Lack, S. D., Lankhorst, N. E., Raye, A., Morrissey, D., & van Middelkoop, M. (2019). Risk factors for patellofemoral pain: a systematic review and meta-analysis. British journal of sports medicine, 53(5), 270–281. https://doi.org/10.1136/bjsports-2017-098890
Selfe, J., Janssen, J., Callaghan, M., Witvrouw, E., Sutton, C., Richards, J., Stokes, M., Martin, D., Dixon, J., Hogarth, R., Baltzopoulos, V., Ritchie, E., Arden, N., & Dey, P. (2016). Are there three main subgroups within the patellofemoral pain population? A detailed characterisation study of 127 patients to help develop targeted intervention (TIPPs). British journal of sports medicine, 50(14), 873–880. https://doi.org/10.1136/bjsports-2015-094792
Manyanga, T., Froese, M., Zarychanski, R., Abou-Setta, A., Friesen, C., Tennenhouse, M., & Shay, B. L. (2014). Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC complementary and alternative medicine, 14, 312. https://doi.org/10.1186/1472-6882-14-312
Espí-López, G. V., Serra-Añó, P., Vicent-Ferrando, J., Sánchez-Moreno-Giner, M., Arias-Buría, J. L., Cleland, J., & Fernández-de-Las-Peñas, C. (2017). Effectiveness of Inclusion of Dry Needling in a Multimodal Therapy Program for Patellofemoral Pain: A Randomized Parallel-Group Trial. The Journal of orthopaedic and sports physical therapy, 47(6), 392–401. https://doi.org/10.2519/jospt.2017.7389
Rahou-El-Bachiri, Y., Navarro-Santana, M. J., Gómez-Chiguano, G. F., Cleland, J. A., López-de-Uralde-Villanueva, I., Fernández-de-Las-Peñas, C., Ortega-Santiago, R., & Plaza-Manzano, G. (2020). Effects of Trigger Point Dry Needling for the Management of Knee Pain Syndromes: A Systematic Review and Meta-Analysis. Journal of clinical medicine, 9(7), 2044. https://doi.org/10.3390/jcm9072044
Ishtiaq, N., Riaz, H., Tahir, M. ., Asghar, Z., Ghulam Rasool, A. ., & Haidar Sial, W. . (2023). Effects of Trigger Point Dry Needling in Patients with Patellofemoral Pain Syndrome; A Randomized Controlled Trial: Dry Needling in Patellofemoral Pain Syndrome. The Healer Journal of Physiotherapy and Rehabilitation Sciences, 3(5), 505–517. https://thehealerjournal.com/index.php/templates/article/view/148
Willy, R. W., & Davis, I. S. (2011). The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. The Journal of orthopaedic and sports physical therapy, 41(9), 625–632. https://doi.org/10.2519/jospt.2011.3470
Petersen, W., Ellermann, A., Gösele-Koppenburg, A., Best, R., Rembitzki, I. V., Brüggemann, G. P., & Liebau, C. (2014). Patellofemoral pain syndrome. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 22(10), 2264–2274. https://doi.org/10.1007/s00167-013-2759-6
Khayambashi, K., Mohammadkhani, Z., Ghaznavi, K., Lyle, M. A., & Powers, C. M. (2012). The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. The Journal of orthopaedic and sports physical therapy, 42(1), 22–29. https://doi.org/10.2519/jospt.2012.3704
Disclaimer: This web site is intended for educational and informational purposes only. Reading this website does not constitute providing medical advice or any professional services. This information should not be used for diagnosing or treating any health issue or disease. Those seeking medical advice should consult with a licensed physician. Seek the advice of a medical doctor or other qualified health professional for any medical condition. If you think you have a medical emergency, call 911 or go to the emergency room. No acupuncturist-patient relationship is created by reading this website or using the information. Morningside Acupuncture PLLC and its employees and contributors do not make any express or implied representations with respect to the information on this site or its use.